Fact sheet 09-2016
M-health for Diabetes Management
Downloadable PDF
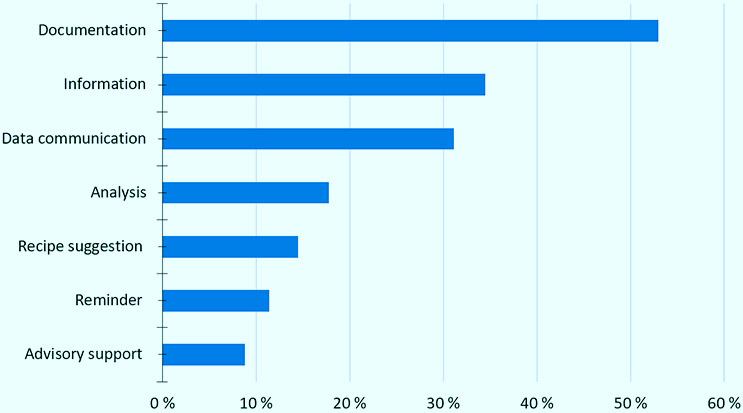
A systematic review in 2014 identified 656 diabetes apps on major app stores [1]. Given the considerable growth of m-health (mobile health) apps in recent years, 57% in 2016 [2], we can expect this number to be even higher by the end of 2016. Although there are a vast number of diabetes apps, the majority offer similar functionalities, and combine only one to two of the following functions in one app: documentation 53%, data communication 31.1%, information 34.5%, analysis 17.8%, recipe suggestion 14.5%, reminder 11.4%, advisory support 8.8% [1].
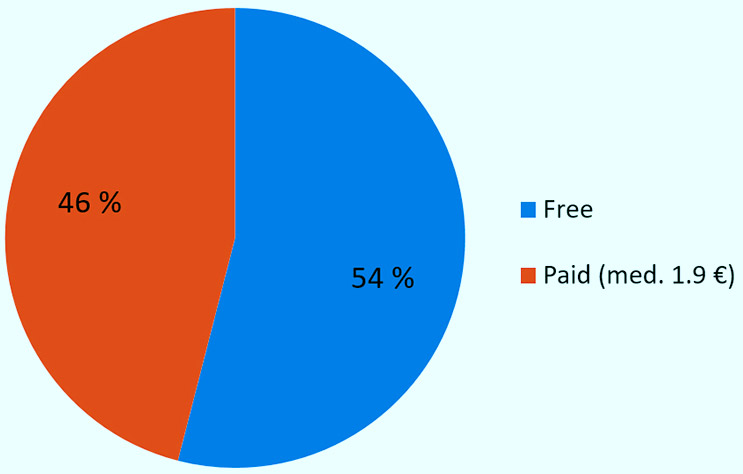
These apps mainly target patients, 96%, and are offered as free downloads, 54%, as well as paid apps, 46%, with the median price of 1.9 € [1].
A recent meta-analysis of 14 randomized controlled trials on the effectiveness of m-health apps in the self-management of diabetes shows a mean reduction of 0.49% in HbA1c for type 2 diabetes studies [3]. This meta-analysis, which is published by the American Diabetes Association, points out that younger patients are more likely to benefit from the use of diabetes apps, and the effect size is enhanced by health care professional feedback.
M-health interventions for diabetes care are not limited to smartphone apps. As a matter of fact, Short Message Service (SMS) has been identified as the most often (40%) used mobile tool in interventions designed for chronic disease management [4].
A very recent systematic review [5], examining the effectiveness of interventions to change lifestyle behaviour delivered via automated brief messaging in patients with type 2 diabetes, identified that there was a difference in HbA1c of -0.53% between intervention groups compared to usual care. This study also discovered that interventions based on unidirectional messages produced similar effects in the outcomes examined, compared to those based on bidirectional messages. Interventions conducted in low- and middle-income countries showed a greater impact than those conducted in high-income countries [5].
References
- Arnhold M, Quade M, Kirch W. Mobile Applications for Diabetics: A Systematic Review and Expert-Based Usability Evaluation Considering the Special Requirements of Diabetes Patients Age 50 Years or Older.J Med Internet Res 2014;16(4):e104.URL: http://www.jmir.org/2014/4/e104. DOI: 10.2196/jmir.2968. PMID: 24718852. PMCID: 4004144
- Research 2 Guidance. mHealth App Developer Economics 2016. Research 2 Guidance. 2016.URL:http://research2guidance.com/product/mhealth-app-developer-economics-2016/. Adgang: 2016-10-26. (Arkivert av WebCite® i http://www.webcitation.org/6lY0vJ78i)
- Hou C, Carter B, Hewitt J, Francisa T, Mayor S. Do Mobile Phone Applications Improve Glycemic Control (HbA1c) in the Self-management of Diabetes? A Systematic Review, Meta-analysis, and GRADE of 14 Randomized Trials. Diabetes Care. 2016 Nov 1;39(11):2089-95.
- Hamine S, Gerth-Guyette E, Faulx D, Green BB, Ginsburg AS. Impact of mHealth Chronic Disease Management on Treatment Adherence and Patient Outcomes: A Systematic Review. J Med Internet Res 2015;17(2):e52. URL: http://www.jmir.org/2015/2/e52. DOI: 10.2196/jmir.3951. PMID: 25803266. PMCID:4376208
- Arambepola C, Ricci-Cabello I, Manikavasagam P, Roberts N, French DP, Farmer A. The Impact of Automated Brief Messages Promoting Lifestyle Changes Delivered Via Mobile Devices to People with Type 2 Diabetes: A Systematic Literature Review and Meta-Analysis of Controlled Trials. J Med Internet Res 2016;18(4):e86. URL: http://www.jmir.org/2016/4/e86. DOI: 10.2196/jmir.5425. PMID: 27095386. PMCID: 4873307