Digital outpatient services - focusing on the person, not the diagnosis
Moving health services home to people can have several positive effects. Researchers are studying patients with different diagnoses, to investigate the usefulness of communicating via an app with healthcare professionals. In this article, researcher Heidi Holmen at Oslo University Hospital and project manager Anna Hurrød in Dignio are interviewed.

Many people who have chronic and long-term conditions are familiar with going to the outpatient clinic for regular consultations. It often involves a long and tiring journey if they live far away from the hospital, in addition to lost earnings.
Once inside the medical specialist's office, the examination can quickly be over, maybe it only takes 15 minutes. The condition is stable, the results from the lab are fine and everything is ok. "See you in three months," the doctor might say. Soon, the inflexible system for physical appointments at the outpatient clinic may be history – at least for some.
«The patients should not have to show up for a physical consultation at the hospital if their health is stable. The aim of the project is to find out how health services can be adapted to people's needs, not the other way around,» says Heidi Holmen.
She is a postdoc and research leader in the clinical study Digital Outpatient Services at Oslo University Hospital. She also works as an associate professor at Oslo Metropolitan University and is a nurse specialized in diabetes.

Since 2020, she and her colleagues have been researching the follow-up of people with epilepsy, cancer, pulmonary fibrosis and pain. Patients with epilepsy, pulmonary fibrosis and pain are recruited for the study from Oslo University Hospital, while people who have cancer and are treated with chemotherapy are patients at the University Hospital of North Norway.
«When we discuss the use of health technology, I am concerned with the users: patients, children, relatives and health professionals. What do patients need and what can they benefit from? How do technological tools affect healthcare professionals' everyday lives and tasks?» Holmen asks.
Will increase quality, safety and capacity in the health sector
The researchers believe that hospital at home will be good for both citizens and those who offer healthcare services. The health authorities are also looking forward to digital follow-up benefiting more people.

Health personnel are a scarce resource, therefore it must be utilized as well as possible. Many hospitals lack medical specialists, which means that patients have to wait a long time for a consultation or treatment.
And every year there are thousands of no-shows – patients who fail to attend their scheduled clinic appointments. This means a waste of both personnel, time and money, which was pointed out in a report from the Office of the Auditor General of Norway in 2018.
Heidi Holmen says it is important to get employees to be positive about trying out technology.
«Healthcare professionals can certainly become positive ambassadors for both colleagues and patients. They can support patients in that it can be a useful tool for communicating with the health service. But to get people to use the technology, it must work well. We must test and adapt the solutions.»

She says that if people manage to use a smartphone, then they will master the technology.
«The most important thing is probably that they must want to learn the new. We should also have room for those patients who do not want or master digital follow-up. Digital services are not necessarily for everyone, but it can be a good alternative for those who want to use it,» says Holmen.
110 patients will test the solution
The thorough research takes time. 110 patients will be recruited and will test the app for six months, while 55 patients have been recruited in a control group. Participants must be at least 18 years old, master a smartphone and Norwegian language, and can not have cognitive impairment. They must have one of the diagnoses on which the solution is tested – even though Holmen says that it is not the type of disease that is most important:
«One goal is to see how this works for many people with different diagnoses. We will measure the effect on generic disease goals such as health literacy, self-rated health and satisfaction with the digital tools. Therefore, we are not so concerned with the direct effect on a particular diagnosis. We believe that the digital follow-up in total will be positive for the individual and their diagnosis.»
Enter info and answer questions
The researchers are collaborating with the health technology company Dignio. In addition, Sykehuspartner, the Norwegian Cancer Society and DIPS, an electronic health record system supplier, participate in the project.
Patients can monitor their health at home via the MyDignio app. They report their measurements, answer questions related to their illness and treatment, as well as results from blood tests taken at the GP’s office. Among other things, lung patients are given tools to perform spirometry tests at home. A change in the person’s health causes a warning to appear on the computer screen of a nurse at the clinic. If necessary, the person is asked to come to a physical consultation.
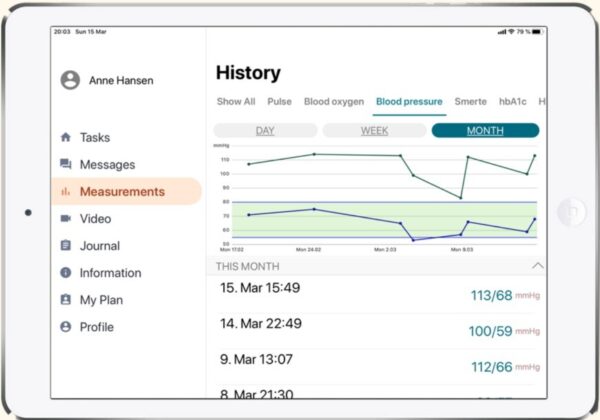
«We ask participants to answer questions about their condition at irregular intervals. For example, a pain patient will be asked if they have pain, and if so, where. A person with lung disease is asked about lung function. Everyone gets customized questions and treatment,» says Holmen.
Data collected from the participants is used for both follow-up and to develop and improve the app.
«Many patients say that they are positive about using the app and that they are looking forward to trying out new technology. While others are unsure whether their digital skills are good enough – and that is something we must take seriously. If you do not master something, that’s important for us to know. Then we must make the solution better.»
Holmen and her colleagues will also interview health personnel about what they think about the Dignio Prevent system, which is the interface used in hospitals. There, health personnel get an overview of patients, state of health and treatment. In addition, they see which measuring devices are integrated with the solution, such as pulse oximeter and temperature meter. In the system, they also receive alerts and messages from patients.
Takes digitalisation one step further
«Our goal is to take digitalisation even further, to reap more positive effects,» says Anna Hurrød.
She is project manager for the Digital Outpatient Services, in the healthtech company Dignio.
Hurrød works closely with Holmen and the rest of the team to improve the interaction between citizens and the health sector. The goal is to use the resources in the health services where they are most needed. Then it is not necessarily the clinic's appointment book that should govern when the patient should see the doctor.
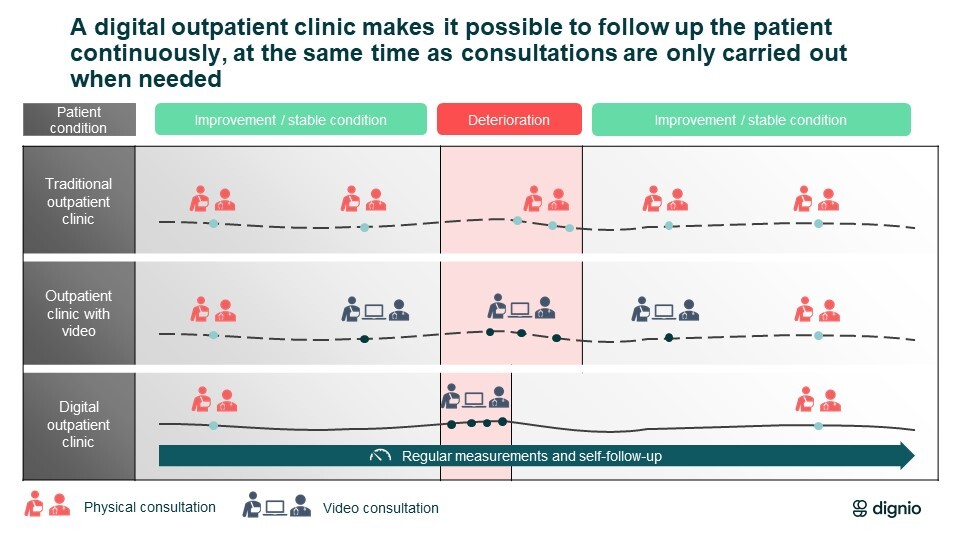
«In some wards, they have become good at offering patients video consultation instead of having to meet physically at the hospital – something that is not always necessary. Video consultation is a good option, but it does not change the process itself or the contact points the person has. We want to change this, so that they are involved in their own health, follow-up and treatment, not least by submitting their own measurements and reporting on their health,» says Hurrød.
She believes we need more innovation and smart solutions in the health sector, to help the steadily increasing numbers of elderly and patients with complex, long-term needs.
«We need fresh ideas and must use more digital tools, because the need for health care is increasing. In addition, citizens are making higher demands. They want insight into their own treatment and want to know what they can do to promote good health and quality of life,» says Hurrød.
Training, workflow, feedback
Recently, she received feedback from the project participants. There was a lot of enthusiasm. Nurses say that patients take more part in what is happening. They see and understand why their health data is valuable and contributes to the treatment.

«The health workers see that they receive more information when the patient reports themselves. For example, a person with epilepsy who does not have frequent seizures will be followed up by the doctor perhaps once a year. In this project, they get questions every three months in the app. If the system detects a deviation in responses from what is considered as normal, healthcare staff will be notified. Then they can ask the patient to come to the clinic and see a health professional.»
Both patients and clinicians must be trained in the system before they can join the study. Patients receive training in using the app at the clinic. Health workers set up the user's profile. Measurements and tasks are added to each user's account. In the hospital wards, several nurses have a key role since they monitor the dashboard in the system. There are also many doctors involved in the project.

«We have discussed methodology, what we want to achieve with the solution, how procedures and workflow should be and how we get a good dialogue with the patient. It is an iterative development and we get frequent feedback from users.»
There is often talk of the untapped potential for health technology products in the health services. Projects and testing are good, but often it is a question of who will pay, so that solutions can be purchased and used.
«I think it is wise to see things in a bigger picture. If each disease is to have its own app, it will be difficult. Solutions that can be used across health care institutions and regions have an advantage. There are often organisational and legal factors that limit the introduction of technology in the health sector. I hope more people want to collaborate across the health sector, since patients and conditions are so similar pretty much everywhere,» says Hurrød.