Closed due to bad weather
The Nordkinn peninsula in Finnmark, in the far north of Norway, is dependent on a road through the mountains. Unfortunately, this particular road is perhaps the road in the entire country that is most often closed due to bad weather.

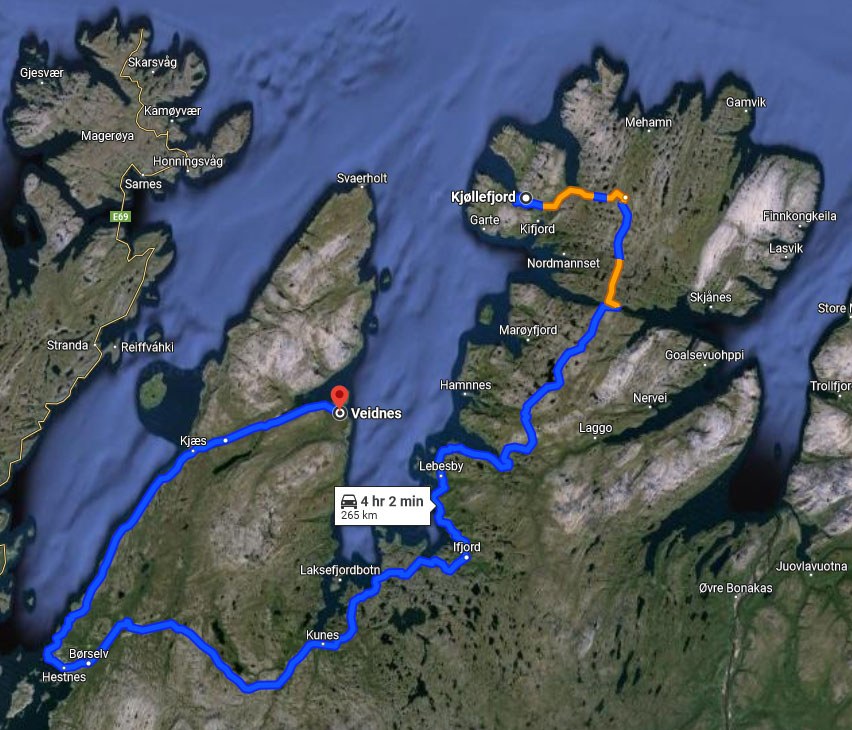
If healthcare worker Simone Wilhelmsen Nilsen needs to drive (and there are no other realistic options) from one end of Lebesby municipality to the other, she must cross not only one but five mountain passes. Round trip it would take her eight hours - assuming she could drive the speed limit the whole way.
One aspect is keeping the roads open. There are often delays due to snow drifts, high winds, and poor visibility. The municipality just does not have enough plows and workers to cover such a large area during a storm.
The other major problem is the quality of the roads.
“When I drive from Bekkarfjord to Veidnes, the road is narrow, bumpy, and has potholes. You do not want to come around a corner at 80 km/hour and run straight into a truck. You have to take it slow,” says Simone.
Simone must always keep an eye out for reindeer wandering down the road. During certain times of the year, roads can close for indefinite periods so that reindeer herds can move between feeding grounds.
Not many people live in the far north of Norway. In fact, there is about one person per two square kilometers in Simone’s area. It is difficult to recruit health personnel to work here. In order to make the most of their resources, the two municipalities that make up the Nordkinn peninsula have to share a midwife and an emergency room.
Despite these challenges, the people who live here deserve and require high-quality healthcare.

A real need for digital remote care
Healthcare workers have trouble providing the same quality of care to patients who live at the outer edges of the municipality. It is not sustainable for them to spend most of their day driving and waiting for the road to open.
Simone is responsible for the remote care technologies in her municipality. Remember how it can take more than four hours to drive one end of the municipality to the other? That’s exactly what Simone must do if someone in Veidnes wants to learn how to use a device or if they need technical assistance. The drive is an investment in that person’s future health and wellbeing.
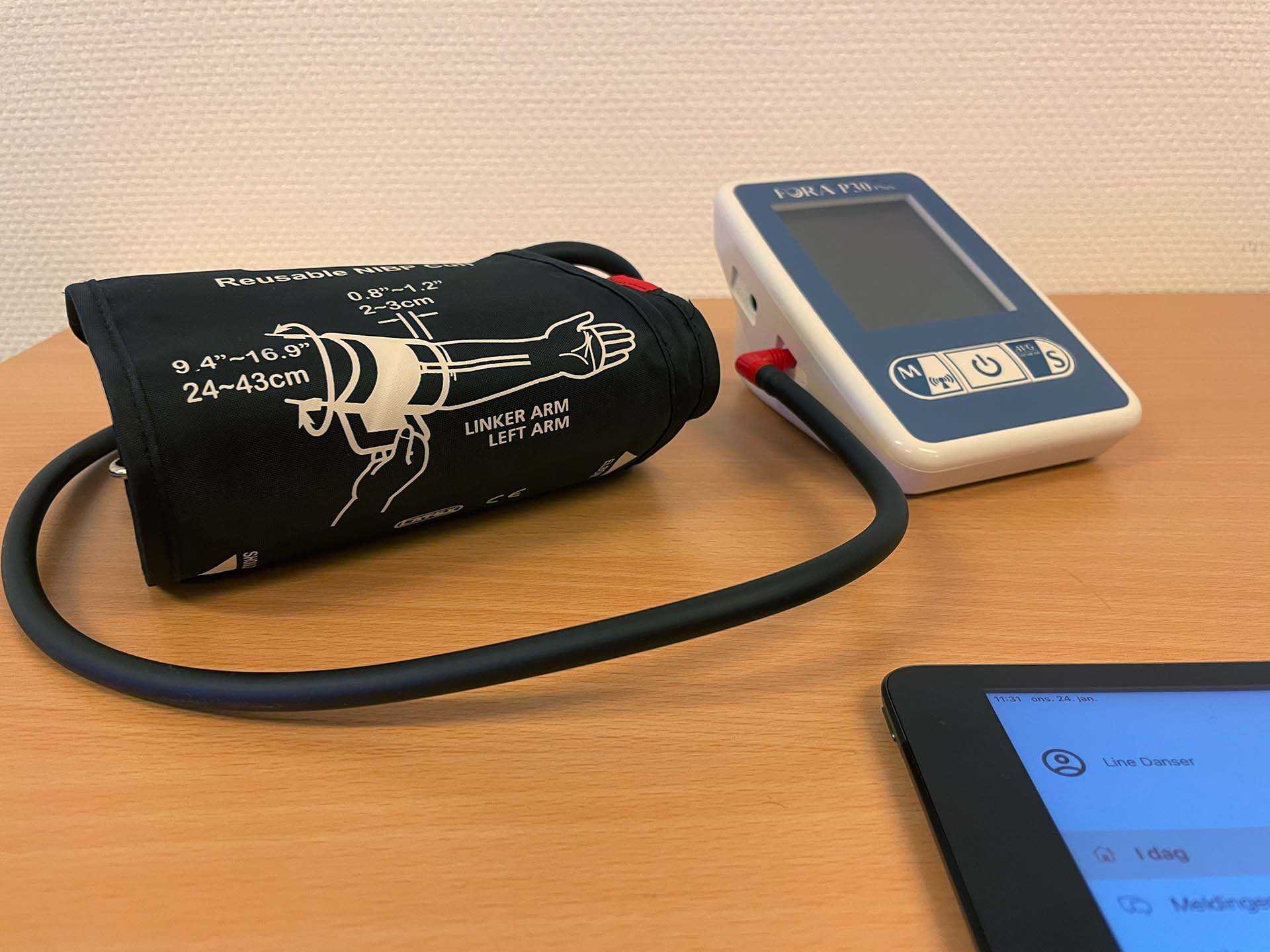
Citizens involved in the remote care program send in their daily health measurements to home care services. They can call or chat with a nurse during regular working hours if they have questions about the measurements.
Digital remote care can cover many different parameters. Lebesby municipality actively uses blood pressure and insulin measurements with remote care patients. They have tested spirometers and thermometers. In the future, they will test how a bathroom scale can be used by patients who need to report their weight to a doctor.
“We purchased oximeters during the Covid-19 pandemic but none of our citizens ended up needing them. For which we are glad,” smiles Simone.
Consultations from afar
In addition to health measurements, the municipality is figuring out use cases for video glasses. Simone describes how the glasses allow health personnel to call each other using Join. Join is Norway’s video platform designed specifically for the healthcare sector. Instead of using a webcam on a computer to show a situation, the glasses are handsfree and allow freedom of movement. You can see the glasses in action for wound treatment here.
In an emergency situation, the glasses could be used to show a patient to a specialist. The medic would discuss the best course of action and be able to start treatment sooner. The closest regional hospital is 30 minutes away by plane, which means that a video call is the fastest way to get an expert opinion. The first medic on the scene might use the glasses to coordinate with emergency services about where to land a helicopter or give an overview of a complex situation.
Video glasses could also be used in planned treatment or consultations. The patient could receive medical assistance locally, rather than having to travel by car, boat and/or plane to the regional hospital. The patient could be at home with a nurse, or at the closest doctor’s office, while the specialist examines the situation through the glasses. Travel in Northern Norway is expensive and time consuming, even more so if the patient needs someone to accompany them.

Quality care, no matter where you live
Not everyone has equal access to doctors, nurses, and specialists. It is especially challenging if you live in a remote location with bad roads and rough weather. Municipalities try to offer as many healthcare services locally as possible, so that fewer patients must make the demanding journey to the regional hospital.
Digital remote care contributes to sustainable healthcare services. Healthcare personnel can be put to use where they are most needed. When the weather makes roads impassable or takeoff impossible, people will still be able to get expert medical advice. Quality and availability of care increase when technology is put to good use.
The goal is to scale up the digital remote care program by including more citizens and a wider range of data that can be monitored. Lebesby municipality would also like to implement self-treatment plans in the future. This would help patients to react accordingly to their daily health measurements and thereby reduce the overall need for healthcare services.
Digital remote care makes it possible for people to live where they want. The upfront cost of the technology and teaching people how to use it is an investment in the future of citizens’ health and wellbeing. A cost that Simone is happy to pay.