3P - Patients and professionals in partnership
There is an urgent call from health organizations, health professionals and health authorities to radically re-design care delivery for patients with long-term and complex needs. Based on the principles of the Chronic Care Model (CCM), the four pilot whole system demonstrators in this project have developed new care models, all of which take advantage of new leading technologies and radical organizational redesign. Our shared vision is a care system which:
- Systematically elicits patient needs, values and preferences translated into health goals, and encourage patient involvement
- Creates an individual pro-active stepped care plan, which communicates: Goals, self-management, dynamic health care plan, action plan for acute episodes and follow-up points
- Has one point of contact for patient's questions and changes in needs
- Has a set of 'clinical response' options, including the recruitment of a seamless inter-professional team
- Provides support for continuous learning regarding key outcomes: Patient goal attainment, patient quality of life and health service utilization
Main Objective
To move safe multidisciplinary care delivery from hospitals towards communities and citizen's homes, while wholly supporting citizens self-management efforts. We aim to validate and verify the prerequisites that support such a 'whole healthcare system' redesign, towards the triple aim of improved -outcomes, improved care experience and reduced costs.
Activities
The 3P project will define, verify, validate and implement pilots in three Norwegian regions and one Danish with the purpose to transform classical profession centric healthcare systems towards citizen centric health service delivery systems in accordance with the above vision. Pilot sites are linked together in a cross-Nordic experience exchange network, an evaluation framework, PhD/ post.doc projects, and a Delphi process which will produce a 'Road Map' for implementation.

The project consists of 10 work packages (WP), of which WP 2-5 make up the four above-mentioned regional innovation arenas and WP 6-10 are research-focused work packages. The four arenas are linked in a learning and research network that will exchange experiences. The latest work package is project management and dissemination.

Final protocol
The 3P research group initially applied for a budget of NOK 50 million, bur the project was allocated only NOK 25 million from HELSEFORSK. The revised protocol with delivery requirements equivalent to NOK 25 million was approved by HELSEFORSK in February 2015. A further set of project changes were made in relation to work package 9 and 10, autumn of 2015.
The final protocol reflects both of the above processes and is appoved by the HELSEFORSK and the Steering Group.
Contacts
- Gro Berntsen, project manager and professor, NSE, email hidden; JavaScript is required
- Undine Knarvik, general manager and senior advisor, NSE, email hidden; JavaScript is required
- Kamilla Michalsen, Financial Advisor, NSE, email hidden; JavaScript is required (on maternity leave)
- Lene Steen Lindseth, Financial Advisor, NSE, email hidden; JavaScript is required
Description of administrative work package
The main task of the project management is to be a driving force for the management of the project, including monitoring the progress in the four innovation pilots (IP), the five cross-cutting work packages (WP 6, 7, 8, 9, 10) and their deliveries, while staying within budget.
The project management reports to the Steering Group twice a year and HEALTHFORSK (source of funding) once a year. We also maintain a set of meeting places within the project to ensure good flow of information between all actors. A good project management is ensured through: a robust project management consisting of three persons who cover scientific, administrative and financial management, together with a project group that has representatives from all the involved regions and partners, and the steering group. The project management is responsible for the development and maintenance of the project page on the web, as a channel of communication towards stakeholders and the public.
Objectives
- Work for a common understanding of the vision of the project
- Ensure financial management
- Ensure follow-up of the work packages and their deliveries
- Support teamwork across project participants
- Contribute to the progress of work packages publications
- Create a network of stakeholders to participate and contribute to the development of a raod map towards a future 3P service
- Ensure the dissemination of the project results and its deliveries to stakeholders and the public
- Ensure implementation of two annual management group meetings, one-two annual workshops / learning networks and a final conference
Learning outcomes 2016
The project management has acknowledged that the creation of a robust project management team, legal cooperation agreements, postdoctoral appointments and securing human resources for the project is a time-consuming process that has been underestimated. Good team spirit, patience and a unique interest in the project among project participants and the steering group has been crucial for today's well functioning team working to meet the goals described above.
Learning outcomes 2017
2017 has shown a good development of the project, both professionally, in terms of communication and in terms of consolidating the cooperation between project participants. The steering group has a constructive approach to the project challenges.
There has been some changes to our original work package structure. Two of the innovation arenas are, or are about to be, completed (Denmark and Stavanger). Nevertheless, we have secured continued contributions from the experienced personnell in the cross-employment package and their participation for the final conference in November 2019.
The representatives of the scientific work packages have found a good form of cooperation with each other, where appropriate. WP 6, 7 and 9 work closely and travel to the innovation arenas (IA) for data retrieval together. WP 8 and 10 work individually and have conducted their own visits to IA.
The project has conducted a Learning Network meeting in Stavanger, November, with participation of about 30 people and a good representation of all work packages, as well as two members from the Steering Group. We have also invited and participated in the National Remote follow-up Project. This is a conscious choice, from the more introvert situation in 2016 where we focused more on internal matters, to an growing ambition of being a resources for national processes and stakeholders.
Using the citizen´s understanding of "what is important to you" as a foundational concept for quality in care is controversial. Understanding how to build healthcare around the citizen poses a challenge. It challenges professionals and the existing health service that has a profession-centered silo organization. This makes the project a forerunner for person-centered care, and the 3P-network is a . strong base for experience-based knowledge on this topic. The 3P network is eager to convey some of this experience in a systematic way through the planned “Delphi” process. We recognize that there are many players around us who are interested in 3P's mindset and that it is urgent to get started the Delphi process. This is confirmed by the project manager's many dissemination assignments in 2017.
Learning outcomes 2018
The project holds a high level of activity. A Learning Network Meeting in Tromsø has been held with 50 participants, and one is being planned and will be held in Kristiansand in October/November with around 70 participants. Knowledge about the project is disseminated in several arenas both nationally and internationally, and there is an increasing interest in the project and its vision. Instead of a Delphi process, we have initiated work towards “a road map for value -added, digitally supported, people-centric, holistic and proactive health service - the 3P Service". Our goal is that this work will ease the communication challenge in providing an efficeint yet precise descriptiono f the 3P-viison amongst stakeholders. The method for this work is under preparation. The scientific work packages are progression well towards ourthe publication goals of up to 10 publications.
Learning points WP 1 – 2019
In the spring of 2019, WP1 has undertaken a "Roadmap" process. 3P has promised to deliver a report advising the Norwegian authorities how to achieve the goal of "a digitally supported, person-centered, integrated and proactive health service for people with complex and long-term needs".
We have chosen to engage a wide group of stakeholders in “road map-meetings” in each of the following regions: North, South, West and East. Invitations are aimed at anyone who works with services for people with complex and long-term needs. We have had between 15 and 40 participants at the meetings.
The roadmap meetings have addressed the following questions:
• What characterizes services that are:
o Person Centered
o Integrated
o Proactive
• What happens if these properties are neglected?
• What is needed to create a service that is person-centered, holistic and proactive in AS Norway?
• What can we do now?
• Evaluation of the meeting. Furthermore, WP1 has followed up reporting to financiers (Northern regional health authorities), follow-up of the work packages in 3P, planning and organization of the learning network meeting in Copenhagen 7-8th of May, and planning of the final 3P-conference in the Spring of 2020.
User reprentative day Tromsø 25.03.2019
On Monday 25.03 the 3P project arranged a workshop on how to strenghten the voice of the user representatives.
We got a visit from Carolyn Canfield, all the way from Canada. She gave a presentation telling her story and how she became a user representative and she gave us some key insight in her work. With that we also got some tools that can be used for user representatives.
Besides Carolyn, Laila Edvardsen (UNN), Kirsti Baardsen (UNN), Solveig Bakken (UIO) og Merethe Krohn (Norges Handicapforbund) held presentations on their work as user representatives. They spoke about how they work, and what are some of the challenges in getting their message across and being taken seriously.
At the end of the day we had a workshop working on how to empower user voice. The day yielded good discusions from the participants and we got many different answers.
Here is the summary of the main points from the discussions:
What does I as a patient need to be a good employee, descion maker and to give good feedback?
- The patients must be heard and taken seriously
- The scientists and other decision makers needs to open their ears and listen.
- Users must be involved from the very beginning so that they can actually be to influence the project.
- Customized information about the research project so that everybody understands what it means to participate.
- Clarify expectation. Important to know what is going on so that you, can prepare.
- Digital platforms makes it easier to provide feedback.
What must we do to support the patient voice and get a greater width in patient voices?
- Important that scientists and others that involve user representatives understand why the representatives should be included.
- It must be a credible project that can "sold" to the patient.
- The researchers have to be honest with the representatives. What is the purpose of the project and what the results are going to be used for.
- Careful with the language used in the meeting with the representatives that is not used to research language. Advantage if there is more than one representative. When you collectively together in the face of a new environment. Recommend at least 3 representatives per project, so that if there is backsliding on a, so can the other two support each other.
- Digital platforms makes it easier to be recruited using the delegate, but can make that some groups are not being recruited.
What is the health professional or health system needs to be able to listen and apply it here the experience better?
- Active relationship to improvement. Ask for feedback and take criticism seriously. Do not go in defense mode.
- Health workers need to have skills in listening.
- Respect for others ' opinions and experiences. Space for religion and faith in alternative therapies.
- Learn from each other wrong. Attitude to accept criticism and praise.
- Easy that the patient voice drowns in all the voices in the health systems. Therefore, one must be aware of to let that voice have an impact in the department.
It has to be something in the systems. What is it we want the systems to contain?
- Feedback to those who provide feedback. This helps to build confidence in the system.
- Improvement culture.
- Space where you can bring up all the possible issues without thinking on the agenda lies behind.
Attached is the presentation from the different presenters.
Merethe Krohn Brukerrepresentant
Laila Og Kirsti Brukermedvirkning Ved Unn
Gode Pasientforlop Solveig Rostol Bakken 2019 En Redigert Versjon
Contacts
- Monika Dalbakk, Project Manager PSHT, UNN, email hidden; JavaScript is required
- Markus Rumpsfeld, Director of Clinic for internal medicine, UNN, email hidden; JavaScript is required
- Lisbeth Spansvoll, Project lead, Harstad UNN, email hidden; JavaScript is required
- Gro Berntsen, Professor, email hidden; JavaScript is required

Description of the innovation arena
The University Hospital Nord-Norge (UNN) has established The Patient Centered Team (PACT) together with the Tromsø and Harstad municipalities. The target population is patients with complex and / or chronic diseases that are at risk for an emergency (re-) admission. The team is interdisciplinary and consists of employees from both municipalities and hospitals working together in a common unit. The team is based on a patient-centered, integrated and proactive approach. PACT coordinates health services for the elderly especially in the transition zone between hospitals and municipalities. PACT makes early assessment of patients at risk of emergency hospitalizations in the municipality and supports discharged patients where there is a risk of re-hospitalization. Patients are followed up by the teams in their homes, municipal institutions and hospitals. The purpose of PACT is the development of better health, patient experience and cost-benefit ratio for this patient group.
Objectives for this innovation arena
PACT is:
- Patient Centered - All decisions are based on what matters to the patient, and then translated into relevant and realistic goals for the health service.
- Interdisciplinary - consists of physicians, nurses, therapists, pharmacists and health secretaries.
- Systematically works in planned cooperation with patient, relatives and relevant health personnel.
- Proactive Preventive focus, prevent development of a clinical crisis, assist usual care in early assessment and diagnosis of at risk home dwelling elderly or hospitalized patients at discharge.
- Mobile - PACT works both in hospitals and in the municipality setting and, assists with planning and follow-up at home after discharge.
The team identifies the realistic, appropriate and necessary measures that will help the patient to reach his/ her goals. Because the team represents both the hospital and the municipality, yet works as a joint team, PACT is able to better keep their focus on what matters to the patient.
PACT helps clarify and secure the care situation where relatives have a particularly heavy care burden. The team also contributes to increased quality of life in a patient's final phase of life. When follow-up plans are implemented, healthcare professionals also feel more secure in the care provided, which ensures continuity of care.
Dissemination - Links and Publications
- Link to UNN website: https://unn.no/avdelinger/medi...
- Article in UNNs internal newspaper: http://www.pingvinavisa.no/vil...
- http://utposten.no/Portals/14/...
- Annual Report 2016
Video:
In the summer of 2018 a video was made with Sigurd Stenersen in Harstad. Here he tells how he
wants to be met by healthcare professionals. Providing correct and safe treatment to the patient at home requires that we change the way we work and cooperate. In a patient-centered health service, we attach great importance to what matters to the patient. The video is produced by the Communications Department of the National Center for E-Health Research.
Learning outcomes 2016
Team members, both in Tromsø and Harstad, find that the teams contribute according to the intentions of the project.
The project is now being piloted in Tromsø municipality, Harstad municipality, and will commence in Balsfjord municipality in 2017.
In 2016, Tromsø municipality had 382 referrals to the team. By 2016, there has been an increase in the number of referrals from General Practitioners (GP) in Tromsø. This is due, among other things, to an active communication strategy towards the GP-offices, and a wide ambulatory activity by the PACT physician. The dialogue between PACT physician and the GPs was intensified, through telephone contact and dialogues.
In 2016, Harstad municipality had 99 referrals to the team. There is still some development work left for both PACT teams, both in hospitals and in municipal health services before PACT can be considered as a fixed part of ordinary health services. PACT experiences that regular contact and exchange of experience between stakeholders helps maintain a good working relationship between different actors in the health care system. PACT has adopted a method of describing the risk picture for each patient. For each patient, a list of "never-events" which the health services adhere to.
Learning outcomes 2017
Positive development. 2017 has been the year in which the patient-centered team, both in Tromsø and Harstad, has become an established contributor to usual care. PACT has incorporated methodology that contributes to a more person-centered, integrated and proactive health service. The PACT service is in line with the project's intentions, within the constraints of today's healthcare organization. The good experiences are a good foundation for new PACT pilots in Balsfjord, Karlsøy and Lenvik.
The need for comprehensive coordination of the health care services for multi-morbid elderly is large. PACT maintains a coordination function across hospitals and municipalities while the patient enrolled in the teams. When it comes to coordination in the slightly longer term, it is difficult to see who in the usual care services take on this task. There is a need for hospitals and municipalities to work together to find common solutions to implement the plans that have been negotiated together with the patient and ensure that the usual care services stay loyal and deliver planned care. The project has accumulated important experience and expertise that can benefit both hospitals and municipalities in the development of the health service towards the ideal of seamless care.
PACT's place in today's system: In the future, there is a need for evaluation and decisions regarding PACT's place and role in today's healthcare system, both in the short and long term. PACT builds a bridge between municipality, general practitioner and hospital. PACT does not take over others' tasks. Nevertheless, there is much dialogue with other units in relation to the division of labour in the patient pathway. Regardless of organizational placement and professional affiliation, it is essential that PACT maintains the ability to work flexibly across organizational boundaries. Flexibility and ability to adjust PACT's efforts based on what matters to the patient and what the next link in the chain of care needs to do a good job is crucial for the effects of PACT-care.
Decision-making processes related to expanding PACT to other municipalities has been challenging. The financial situation in both hospitals and municipalities has led to an increased expectation of impact assessment and realization of benefits before new measures such as PACT can be disseminated . Preliminary research results have been presented to the "owners" of the PACT intervention in both municipalities and hospitals in support of the decision-making process. These have been useful to decision makers, but have not led to final clarifications.
It is demanding to use even unpublished results for such purpose. This process has revealed management needs for continuous monitoring and publishing of accurate otucome results that can guide the decision making process, making the decision-making process transparent and knowledge-based. However, the research process is neither designed nor has the resources to deliver results in line with these needs.
Learning outcomes 2018
1) Transition from project to being part of usual care in Tromsø:
PSHT has now been a pilot project in Tromsø for 3 years. PACT is well established. While the PACT method is well established, it still undergoes a continyous improvement process. From January 2019 PACT will be an operational part of usual care in Tromsø. During the project phase, PACT has access to both the municipal and hospital records under a "quality assurance clause" in the Health Personnel Act. When PACT now becomes operational, it is unclear if such sharing of records can continue under today’s legislation.
2) Decision-making process in Harstad municipality.
Harstad municipality has been unsure of whether PSHT should be part of the municipal care services. Harstad has prepared their own evaluation of PSHT, which is underway.
3) Extending PACT to Lenvik municipality. Lenvik will also become a PSHT municipality. Lenvik has a decentralized center for specialist care, and has also been chosen as a model municipality for the government's piloting of multi-professional care teams. The organizational model for Lenvik needs to take these organizational units into account when the Lenvik PACT team is designed. 4) PACT has received a lot of attention from the groups outside the region in the last six months. We have presented both the PACT model and results for decision makers at a number of venues at national and regional levels.
5) Dissemination of the PACT principles in both hospitals and municipalities. Because of the good results PACT, the regional health authorities and the University hospital are considering how to use the PACT formulae in a wider context, and to improve the socio-technical approach to PACT.
6) The publishing process. The paper that describes the initial PACT results was not accepted for publication by the larger general medical journals. The PACT paper is now under review in BMC health services research.
Learning outcomes spring 2019
The innovationarena in the Northern health region has experienced an adventurous growth in interest. From a bit of curiosity in 2018, the project team has now become "travelers in Person-centered, holistic and proactive services". Markus Rumpsfeld, is challenged to develop health services that target all people with complex and long-term needs in the University hospital of Northern Norway’s (UNN) uptake area. The project has been named: The «SuperUser project». The new hospital in UNN Narvik becomes the first site in the "Super User" project.
This is now a program consisting of 4 parts:
• Service innovation - new services
• Organizational development - dissemination of existing services
• Technology and e-Health - Digital support
• Interaction - internal and external - agreements on interaction with external actors outside the specialist health service
The original innovation arena: Patient-centered Team (PACT), continues and is now moving from project to operations in both Tromsø and Harstad municipalities. We are still in a project phase with Balsfjord, Lenvik and Karlsøy municipality. Lenvik municipality is also part of the health authorities "follow-up team-project". UNN and the municipalities surrounding it have decided that PACT should be disseminated to all UNN municipalities.
Care innovations and agreements of who does what when across the hospital and municipal services.
Building capacity to improve care for persons with CLNs together with the regional teaching institutions.
Supporting development and implementation of digital tools for persons with CLNs. Essential is health analytics to identify and flag the person with CLNs, a shared digital plan, and support of virtual care delivery.
The national 1C1EHR goal for an interoperable open data platform builds on the national e-health portal (HelseNorge.no) which provide several patient-facing tools (access to my EHR, medication lists, general health information etc) and interoperability tools (IHE – XDS, the digital care plan) which support sharing of documents and plans across care organizations. The latter are expected in 2020-21. Also important is the configuration of structured information elements (archetypes) in an ongoing national effort, which will ultimately enable flexible design of information flows and new care pathways. Implementation of DIPS will be incremental and iterative by clinic.
Contacts
- Wenche Tangene, Project manager and Senior advisor, Research Department (FOU) Sørlandet Hospital HF, Kristiansand, email hidden; JavaScript is required
- Frode Gallefoss, Research director, Sørlandet Sykehus, Professor, dr. med., K2, University of Bergen, email hidden; JavaScript is required
Description of the innovation arena
Project Manager: Sørlandet Hospital HF
Collaborators: The University of Agder (Department of Information and Communication Technology) and Risør Municipality, which is the local innovation arena.
Brief description of the service: Telemedicine follow-up from the telemedicine center in Risør municipality and the formation of an interdisciplinary team with the patient as a central member of the team. The target group is patients with COPD who have acute or chronic deterioration of the disease. There is an opportunity for inclusion of other groups of patients at a later date.
Objectives for this innovation arena
The project goal is to describe how telemedicine follow-up of patients is integrated in collaboration with interdisciplinary teams. The most important factors to measure in this context is the patient’s sense of empowerment and security.
Main hypothesis for the innovation arena: "Telemedicine follow-up of patients with COPD increases patient empowerment from start-up to 4 weeks after established treatment, providing increased patient safety. Sense of empowerment is evaluated at the start-up and after 4 weeks follow-up via tablet. Sense of security is evaluated by 4 weeks of follow-up. »
Secondary goals: The innovation arena (Risør municipality) will consider possible organizational changes due to telemedicine and the establishment of primary medical teams.
Inclusion: Continuous inclusion of patients with acute or chronic COPD aggravation that may receive adapted telemedicine equipment. In addition, inclusion of patients with COPD in need of telemedicine follow-up, these are recruited from GPs and specialists.
Target number of inclusions: Inclusion of at least 15-20 patients included in the study and follow-up for at least 1 month.
Dissemination - Links and Publications
Risør municipality is also a partner in the TELMA project - a major telemedicine project in which Kristiansand municipality is a project owner and collaborates with Farsund Municipality, Risør Municipality, Sørlandet Hospital Kristiansand and the University of Agder. Both projects are successors of the United Kingdom Telemedicine project United4Health, which was completed in 2015. The overall objective of TELMA is to develop a common telemedicine solution for the entire Agder.
Smaradottir Berglind, Fensli Rune, Naley Ås Inger-Alice, Gallefoss Frode. Telemedicine follow-up of Chronic Obstructive Pulmonary Disease Integrated into a Patient-Centric Health Care Team Setting-Impacts on Patient Empowerment and Safety Published by the IEEE Xplore Digital Library in 2018.

Berglind Smaradottir presented this paper at the conference Computational Science and Computational Intelligence (CSCI’17) in Las Vegas, USA. The paper describes the research agenda and research plan for work package 3.
Smaradottir presented in May 2018 an abstract at the conference «Teknologi i Helse og Omsorg» at the Western Norway University of Applied Sciences in Bergen.
In September 2018, Smaradottir has visited the University of Copenhagen for a study trip on the eHealth literacy questionnaire that is used in work package 3.
Research WP 3:
The project group has submitted a paper in April 2019 to the Journal of Care Research (Tidsskrift for omsorgsforskning), targeting the experiences regarding the telemedicine follow-up in Risør.
Learning outcomes 2017
Telemedicine solution and data storage: There have been discussions, ambiguities and partial disagreements about whether the data storage solution meets the Norms (Information Security Information) requirements for information security. It has been decided that project owners for the TELMA project (Kristiansand municipality) have procurement and system responsibility for the solution. Project participants who deliver data to the supplier of the solution are each required to sign a data processing agreement with this supplier. By the end of 2017, a new technology platform for telemedicine follow-up was implemented and the solution meets the requirements of the Norm for Information Security.
Technological challenges: The telemedicine follow-up is now made by Kristiansand telemedicine centre.
Constraints: The 3P project has been dependent on progress in the TELMA project. Deadlines that have been shifted in TELMA have led to displacement also for 3P. As a result of clarifications related to technological solutions, in 2018, full focus will be on the inclusion of new patients in the project.
Collaboration: In conjunction with several months' disruption of start-up date, the agreement with the hospital in Arendal has received a completely different level than previously proposed. In the first half of 2018, a review will be made of how the hospital can take a role in the project as part of the interdisciplinary team to follow up the patient. Today the follow-up in Risør municipality is closely linked to the home nursing rehabilitation team. In 2018 efforts will be directed at involving the patient’s GP when new patients are included in the project.
Learning outcomes 2018
At the beginning of 2018, Risør municipality evaluated the experiences with the telemedicine centre. The conclusion was that that the operation of the telemedicine centre was vulnerable because of the challenges regarding staff and in periods there was lack of competence to operate the centre in a proper way. Different solutions were discussed, but they were not realizable within this project. After internal discussions and evaluations in Risør municipality and the project group of Helse SørØst, it was decided to make an agreement with the TELA project and the Telemedicine centre at Valhalla to carry out telemedicine. The agreement was signed in Mai 2018 and the first patient included in June 2018. For different reasons, the start of the telemedicine follow-up was in September 2018. There are today 2 included patient that have telemedicine follow-up.
It has been a challenge to recruit patients to the project. It was experienced that patients that could benefit from telemedicine follow-up often do not receive other municipal health services, therefore the inclusion of patients must be referred from General Practitioner (GP) or the hospital. Regarding the GPs, there have regular meetings and they are informed, but anyway there has been limited recruitment from them. No patients have been recruited from Arendal hospital, and that is probably one of the reasons the low numbers of inclusion.
Risør municipality has developed routines for collaboration with the GPs. The home nursing services have meetings with the GPs every 6th week, and there is close collaboration and communication with the GPs regarding each patient. In addition, the municipality has administrative meetings with the GPs. For patients that are referred from the hospital, the GPs are contacted with an e-message and they collaborate during the telemedicine follow-up.
Contacts
- Kenneth Austrått, Project Manager, email hidden; JavaScript is required
- Heidi Grundt, Lead Researcher, email hidden; JavaScript is required
Description of the innovation arena

The pilot site is carrying out a randomised controlled trial (RCT), for patients with a chronic obstructive pulmonary disease (COPD) and FEV1 < 50 %. Patients receive a tablet and a pulsoxymeter when discharged from hospital after a COPD- exacerbation. They’re randomised into three different groups: follow-up by tablet (video consultation), by phone calls, or no intervention. Over a period of 14 days, they get information about the self-management of the disease and they are monitored daily by automatically transferred data from pulsoxymeter (O2 and pulse).
A report (link under “reports”), written by SINTEF, at potensial service models for Helse@Hjemme (Health@Home). This report were made in collaboration with different municipalities, patients and other actors in the existing service model.
The project finalized inclusion of patients by March 2018, and a six and 12 months follow-up of the patients. Data from follow-up is now collected and being investigated.
Objectives for this innovation arena
The site’s primary goal is to finish the RCT study, and further bring knowledge on how to find a better method to follow up patients with COPD.
Dissemination - Links and Publications
Web page (Norwegian): https://helse-stavanger.no/avd...
Saleh, S., Larsen, J. P., Bergsåker-Aspøy, J., & Grundt, H. (2014). Re-admissions to hospital and patient satisfaction among patients with chronic obstructive pulmonary disease after telemedicine video consultation - a retrospective pilot study. Multidisciplinary Respiratory Medicine, 9(1), 6. http://doi.org/10.1186/2049-69... Link: https://www.ncbi.nlm.nih.gov/p...
Reitan, J., Halvorsen, T., & Svagård, I. (2016). Samhandlingsmodeller for avstandsoppfølging av kronisk syke. Trondheim: SINTEF.
Learning outcomes 2018
Collaboration with the primary health care: The governmental Department of Public Health awarded the Municipality of Stavanger the role of a national pilot for remote follow-up for patients with chronic illness. Helse@Hjemme was a partner in this application, and worked together with the municipality of Stavanger to develop a method for the follow up of these patients, based on their needs and interests. Stavanger University Hospital carried out a study to find an optimal way of following up patients, which would outline which service level should provide services to the the patient at specific times (see report below, only in Norwegian).
The municipality of Stavanger is project owner , and now has the responsibility for follow-up of patients, and technical devices in the pilot project. During the work with service design, it became clear that the primary and secondary care levels, had different interests and skillsets, both necessary for the implementation of a good service design. For this reason: Helse@Hjemme is now a member of the reference group of the national pilot.
Development versus study: Helse@Hjemme is carrying out a randomised controlled trial (RCT), of COPD patients after COPD exacerbation and other detailed conditions.
This study method has clear limitations, even though the data from the RCT-intervention give important input for development of new service models for patients with a chronic illness. The study will only be an input to a service model, and not an actual service. Interest from other municipalities: Several municipalities considered the opportunity to combine telemedicine, for patients with complex and longterm needs (CLNs) , with the more general safety alarms service. 13 municipalities in the county of Rogaland, under the leadership of the municipality of Sandnes, tried to develop a way to collaborate on how to follow-up both elderly and patients with CLNs. The group has tested both a centralised and a decentralised solution. Stavanger University Hospital has contributed to this work, inter alia with experiences from Helse@Hjemme. The report is available here.
Contacts
- Klaus Phanareth, MD, PhD, Epital Health A/S, email hidden; JavaScript is required
- Søren Vingtoft, MD, Senior consultant e-health, Epital Health A/S, email hidden; JavaScript is required
- Lars Kayser, MD, PhD, e-health specialist, University of Copenhagen email hidden; JavaScript is required
Description of the innovation arena
Epitalet has been operating as Living Lab since 2012 in the Lyngby-Taarbæk municipality. During this period, Epitalet has developed and tested a person-centered health care model where citizens with serious chronic diseases are digitally linked to a network of health professionals. The network is based on a self-monitoring and proactive self-management approach to prevent acute and sub-acute deterioration. Epitalet has developed a response and coordination center, where the nurses at the response center contact users through digital video and online tools. The response center also consult e-doctors to initiate treatments, as well as a mobile emergency team consisting of health professionals who are sent out to the patient's home when needed.
The Epital Care Model (ECM) is now published in JMIR (see below). The model is based on the following healthcare declaration:
"Citizens Telemedicine Manifesto"
1. Vision
- Create security
- Promote quality of life
- Avoid hospitalizations
2. Mission (System Requirements)
- Availability (24/7, 365)
- Response time to citizen calls (<5 minutes)
- Mobility (global connectivity)
- Patients are co-producers of care (empowerment)
- Stability (budget security)
3. Equipment and services
At Home with the patient:
- Online clinical measuring devices
- Internet and communication equipment with video
- Emergency medications available at home in medicine box
At the response center:
- 24-hour staff with trained personnel
- E-doctor consultation support the front line personnel
- Mobile Acute emergency team
4. Organizational framework
- One contact point for the citizen
- Clarity regarding the responsibilities of every contributor
- Active citizen network for COPD and chronic diseases
- Robust buy-in in the health sector
- Approval from regulatory authorities
- Ensuring further co-production together with citizens
Dissemination - Links and Publications
"Epital Care Model (ECM)":
Scientific publication of the Epital Care model:
http://www.researchprotocols.o...
TED talk from 2012:
TV2 Lorry show from 2014 (in Danish):
http://www.tv2lorry.dk/nyheder...
Video for ECM 1 - Independent and Active Living from 2010:
WP 5, Innovationsarena Epitalet, has given inspiration to expand the ECM (Epital Care Model) test in Odsherred municipality in Region Zealand. This happens as part of the PreCare project (https://innovationsfonden.dk/) which will establish an e-clinic in 2018 as a missing link between Holbæk Hospital and Odsherred municipality's GPs and the municipality's health functions. In this context, cooperation between 3P and WP 5 will be expanded and strengthened. Region Zealand will therefore be involved in the cooperation with and experience exchange in 3P in the future.
Vision video for ECM 4 ("Out-mitted at Home") from 2010:
Learning outcomes 2018
Epitalet is in the process of establishing a new "Whole System Demonstrator" in Odsherred municipality in collaboration with Region Zealand and Holbæk Hospital based on the experiences from Lyngby-Taarbæk municipality. The starting point was the start of the PreCare project in early 2018, which should explore opportunities for more proactive services within the existing healthcare system.
During the first 6 months of the project it became clear that the use of the ECM model should be used as a reference model in order to create a real person-centered healthcare based on ECM principles. Subsequently, the possibilities were investigated to establish coherent ECM functions in the existing organization, either within the hospital or as an extension of the municipal health functions. None of the parts proved to be possible and after the summer 2018, it was decided to establish a whole new organizational unit – the eClinic – which would act as a legal independent medical organization with instructional powers over nurses employed in Odsherred municipality and with cooperation agreements with Holbæk Hospital and the municipality's practitioner doctors.
Following this, an infrastructure of the eClinic has been established, which includes:
- Development of an ECM journal in collaboration with Appinux
- Establishment of a "point of care" laboratory in collaboration with Radiometer
- Collaboration with device suppliers (Spiromagic).
The eClinic is in the process of establishing the following functions:
- Response and Coordination Center (RKC) – (ECM2-5)
- Mobile Emergency Nursing Care Team (MAS) - (ECM3-4)
- Municipal Acute Pathways - (ECM 5)
With this set-up, we plan to offer citizens with COPD a 24/7 telemedicine service and citizens with acute deteriorations within 31 internal medical diagnoses can be examined and treated by the staff of the eClinic (nurses and e-doctors).
One of the objectives of the eClinic is to reduce the incidence of acute hospitalizations from Odsherred municipality by 30% over the next year.
Contacts
- Rune Fensli, Professor og forskningsleder. Senter for eHelse, Universitetet i Agder, Grimstad. email hidden; JavaScript is required
- Berglind Smaradottir, Researcher, Research Department, Sørlandet Hospital HF, Kristiansand. email hidden; JavaScript is required
Description of the Work Package
The main goal of work package 6 is to map and evaluate the technical solutions that are used by the inter-disciplinary health care teams at the four innovation arenas. The focus is functionality, usability and organisational aspects regarding the use of the technical solutions, and how they support team collaborations both internally and between organisations. Berglind Smaradottir has been employed from the 1st of January 2017, in a 50% position as a researcher at SSHF, with the main response for the research in WP 6 together with Professor Rune Fensli at University of Agder. She will also contribute with research in WP 3.
Objectives
WP6 has the aim to evaluate the situation «as is» and also how the interdisciplinary health care team propose the solutions of the future «to be». The mapping is mainly based on qualitative methods with observations and interview with key informants at each innovation arena.
Dissemination - Links and Publications

B. Smaradottir, R. Fensli. The Technology Use and Information Flow at a Municipal Telemedicine Service. Stud Health Tech Inform 251 (2018), p. 293-296. The paprer is an evaluation of telemedicine technology in Risør. Open-Access & Medline-indexed: http://ebooks.iospress.nl/volu...
B. Smaradottir, R. Fensli. Evaluation of a Telemedicine Service Run with a Patient-centred Care Model. Stud Health Tech Inform 251 (2018), p. 297-300. The paprer presenting the arena Lyngby-Taarbæk and the evaluation of a telemedicine solution for COPD patients. Open-Access & Medline-indexed: http://ebooks.iospress.nl/volu...
B. Smaradottir, R. Fensli. A Case Study of the Technology Use and Information Flow at a Hospital-driven Telemedicine Service. Studies in Health Technology and Informatics 2017:244, p.58-62. Available at: http://ebooks.iospress.nl/volu... (Medline-indexed) DOI: 10.3233/978-1-61499-824-2-58. The paprer describing the arena in Egersund (Helse@hjemme) where the technology and information flow was evaluated.
B. Smaradottir, R. Fensli. Evaluation of the Technology Use in an Inter-disciplinary Patient-centered Health Care Team. Stud Health Tech Inform 257 (2019), p. 388-392. This paper presents the evaluation of the technology support at patient-centered health care team at University Hospital of North Norway. Open-Access & Medline-indexed: http://ebooks.iospress.nl/volu...
B. Smaradottir, R. Fensli. Integrating Care Through Patient-centred Health Team Working across Organisational Borders. Studies in Health Technology and Informatics 2017:244, p.85. doi:10.3233/978-1-61499-824-2-85. Available at: http://ebooks.iospress.nl/volu...
This is a short paper/abstract from an early project phase in WP6 and it was presented as a poster at MIE2017 in UK.
Two papers have been accepted about patient experiences and user experiences regarding technology, to be published in July and August. One paper is under review at Elsevier.
Smaradottir will present together with Ståle Sjaavaag at eHelse2019 in May in Oslo. Topic: experiences from the arena in Risør and research in 3P.
Smaradottir participated at eHelse2018 and presented together with Kenneth Austrått at Stavanger Universitetssykehus the results from the innovation arena in Egersund. eHelse 2018 was organised by the Norwegian Computer Association, the Norwegian Medical Association and the Norwegian Nursing Association in Oslo, April 2018.
Smaradottir participated at EHIN2017, eHealth in Norway national conference, and had a presentation based on WP6 in 3P at the Research track. EHIN had more than 1000 participants.
Learning outcomes 2017
In the beginning of 2017, an application to Norwegian Centre for Research Data (NSD) regarding approval of data collection and storage of research data.
Berglind Smaradottir and Rune Fensli have made four visits to the innovation arenas together with WP 7 & 9 in Egersund, Tromsø, Lyngby and Risør. Interviews, mapping of communication processes and observations were made during 2-3 days at each arena. We experienced that two days was to short time, and there was need for more time at each area, as several researchers wanted to interview the same informants. Berglind has later made visits to Egersund and Tromsø to complete the data collection with more interviews. A visit to Risør in was made in January 2018 to observe and evaluate the technology.
Learning outcomes 2018
“We are closing the data collection, analysing data and writing one final paper to summarise the results for WP 6 and providing recommendation for the future.
Contacts
- Lars Kayser, MD, PhD and e-health specialist, University of Copenhagen, email hidden; JavaScript is required
- Eunji Lee, Postdoctor, OUS/University of Copenhagen, email hidden; JavaScript is required
Description of the interdisciplinary work package
The main focus of the work package is clinical documentation and evidence in collaboration with patients with chronic disease. It will provide a basis for understanding how to address the patients' health literacy, digital health literacy and empowerment in the long run.
The purpose of Work Package 7's contribution to the project is to map guidelines and best practice in dealing with people with one or more chronic conditions. Furthermore, the work package should provide suggestions for how clinical interactions can be supported by digitally. It is initially focused on people with COPD. Later it will focus on people with diabetes and cardiovascular disease, as well as other chronic diseases.
We aim to map to what extent there are literature, guidelines and recommendations in these thematic areas in Norway, Scandinavia and other countries.
Furthermore, we will look at how consultations and interactions take place in practice, and what barriers and challenges that arise in connection with the implementation of clinical guidelines across sectors.
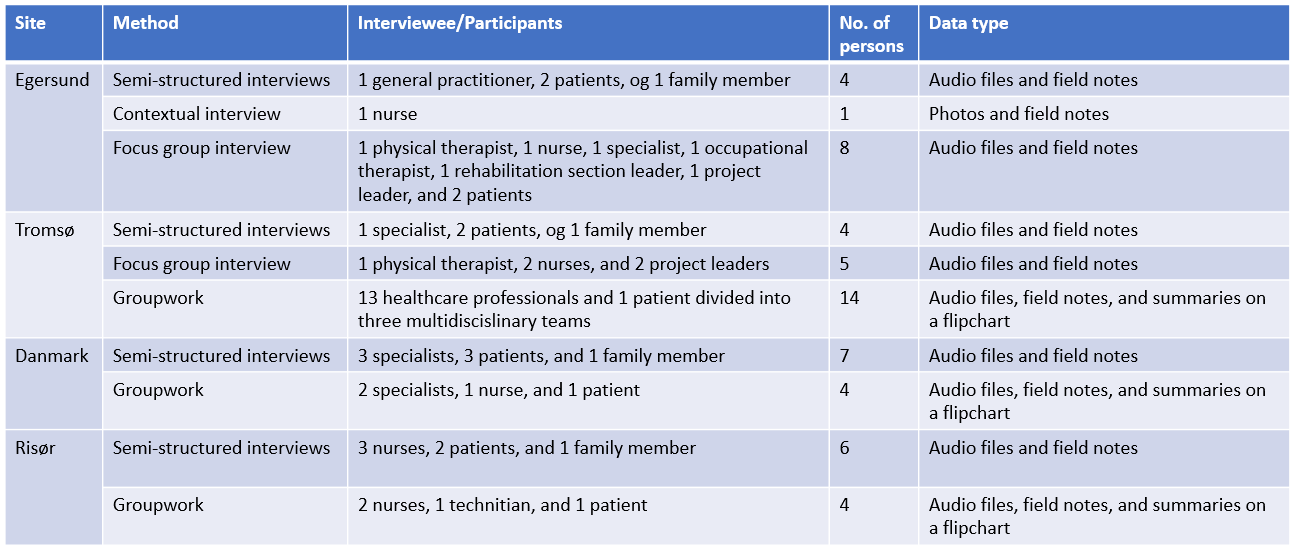
Completed data gathering activities 2018 for WP7 and WP9 (fieldwork)
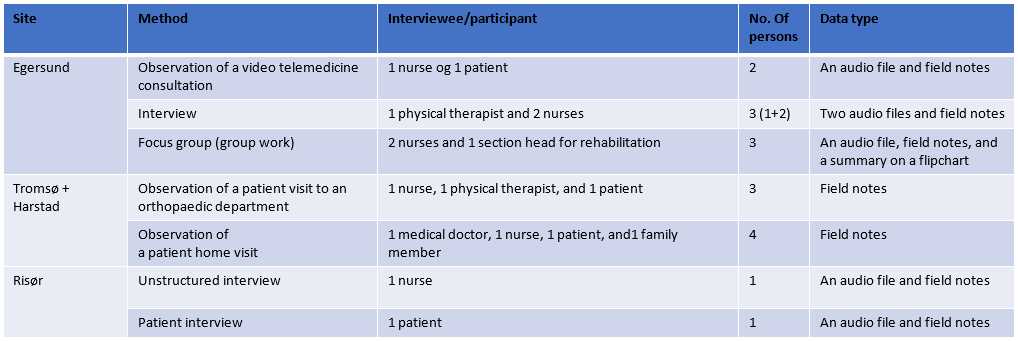
Completed data gathering activities 2017 for WP7 and WP9 (fieldwork)
Dissemination - Links and Publications
Eunji Lee, Lars Kayser, Deede Gammon and Gro Berntsen. Engaging and empowering citizens with long-term conditions: How to define personal goals and how to support the goal achievement with technology? The 18th International Conference on Integrated Care (ICIC18). Link to abstract:
https://drive.google.com/drive/folders/1G6QO4yTFb5wJEk9xEvRHtcZn4Ly8YYZk
Learning outcomes 2016
The projects we investigate in the field have changed the scope and the organizations. It is therefore difficult to fully disclose all aspects of each site. We need to work with both historical and current perspectives.
The four innovation arenas will together contribute to our learning, so it's important to combine these experiences.
Learning outcomes 2017
WP 7 works closely With WP 9 because the patient's individual digital plan in WP 7 must be adapted to the patient's goal (WP 9). WP 7 and 9 are covered by a joint post doc. Post doc E. Lee was employed in spring 2017. The postdoc and the WP leader have visited four of the innovation arenas and published an article on a service design approach that we tested in a visit to Tromsø.
We design data collection activities linked to patient goals and digital support. For example, we held group work with both healthcare professionals and patients. We discussed first 1) What is important in the patient's life? And 2) What kind of clinical data is important to gather and share to support follow-up of the personal goals identified in the first question.
We are launching a literature search on "How personal goals in people with chronic diseases can be formulated and followed by information and communication technology. This will be an article published later this year.
Learning outcomes 2018
The preliminary impression from fieldwork on individual care plans:
- Telemedicine remote monitoring seems to work well (Egersund and Risør).
- The teams are not able to access the patient's data from a GP/emergency care, which makes it difficult for them to get the overview of patient journey (Tromsø and Harstad).
Preliminary findings from scoping review on digital support for personalized health goals and individualized care plans. Full-text screening is now underway.
- Main care plan disease types: type 1 or 2 diabetes, COPD, cardiovascular disease/failure, mental disorders, uncontrolled blood pressure, and cancer.
- ICT Communication support for careplans: telephone call, mobile app, video conference, text message, website (portal, software, etc.), wearables, email, face to face, and PDA program.
Contacts
- Kari Dyb, senior researcher, Norwegian Centre for E-health, email hidden; JavaScript is required, tel +4790110922
- Lisbeth Kvam, forsker, NTNU, email hidden; JavaScript is required, tel +4773559357 and +4799241349
Description of the Work Package
Redesign of care is a complex intervention. Many promising technological innovations in health and social care are characterized by nonadoption or abandonment by individuals or by failed attempts to scale up locally, spread distantly, or sustain the innovation long term at the organization or system level (Greenhalg et al 2017). The active ingredients in implementation processes are multiple, interacting and context depending. Hence, there are a number of factors associated with implementation results. WP 8 focus on implementation and deployment processes from the perspectives of health care providers. The empirical settings are four different health-technology initiatives, three in Norway and one in Denmark, who share the “3P-core vision about truly citizen centred care”. We will especially examine effects of fidelity to the 3P care vision on results and are particularly interested in the ways that ideas about the value of patient care as a craft are deployed to frame new technology-supported practices, and how this value potentially contest and support the legitimacy of the intervention.
Objectives
- Produce new social science knowledge on implementation of complex interventions in health care, including an evaluation framework based in existing implementation theory: NASSS: Nonadoption, Abandonment, and Challenges to the Scale-Up, Spread, and Sustainability of Health and Care Technologies (Greenhalgh et al 2017).
- Use the evaluation framework to support the implementation of the 3P productive teams intervention with rapid feed-back cycles.
Research questions
- How are the 3P visions and values concerning patient care materialized and communicated in day to day practice at the different innovation arenas?
- How does the 3P vision about technology-supported citizen centred care relate to other contemporary visions and values of patient/citizen care as a craft?
Dissemination - Links and Publications
Andreassen, H. K., Dyb, K., May, C. R., Pope, C. J., & Warth, L. L. (2018). Digitized patient–provider interaction: How does it matter? A qualitative meta-synthesis. Social Science & Medicine, 215, 36-44. Main points of the article: When patient-professional relations are digitized, relations are respatialized, and there are reconnections of relational components. These lead to empirically specific reactions, which can be characterized as reconstitutions and renegotiations of social practices, which in turn are related to the reconfiguration of basic social institutions. We propose a new direction for exploring the digitalization of health care to illuminate how digital health is related to contemporary social change.
Work in progress: Adoption or Non-adoption - Money Talks: A qualitative analysis of the implementation of four technology supported Patient Centred Care initiatives.
Visions in practice: Patients and professionals in productive teams. An implementation study from Scandinavia. Evaluation framework for rapid-cycle feed-back on the implementation processes.
Learning outcomes 2018
We have published one scientific article.
Good response on the rapid feedback to users in Tromsø 2017 and Stavanger 2017, here, we developed an evaluation framework based on Normalization Process Theory (NPT).
We have conducted fieldwork at all the innovation arenas, in Norway and Denmark and are in the process of data analysis and writing papers.
Learning outcome spring 2019
At the end of 2018, the paper “Digitized patient–provider interaction: How does it matter? A qualitative meta-synthesis” was published in Social Science & Medicines. The paper is a result of a long-standing social science collaboration between 3P researchers; Hege K. Andreassen and Kari Dyb, the two British sociologists; Carl R. May and Catherine J. Pope; and Line L. Warth from Norwegian Centre of E-health Research. Abstract included:
In this paper, we present a meta-ethnography of 15 papers reporting qualitative studies of digitally mediated patient – professional interactions. By dissecting the detailed descriptions of digitized practices in this most basic relationship in health care, we explore how these studies can illuminate important aspects of social relations in contemporary society. Our interpretative synthesis enables us to reassert a sociological view that places changes in social structures and interaction at the core of questions about the digitization of health care. Our synthesis of this literature identifies four key concepts that point at structural processes of change. We argue that when patient-professional interactions are digitized, relations are respatialized, and there are reconnections of relational components. These lead to empirically specific reactions, which can be characterized as reconstitutions and renegotiations of social practices which in turn are related to the reconfiguration of basic social institutions. We propose a new direction for exploring the digitalization of health care to illuminate how digital health is related to contemporary social change.
In this paper, WP8 address an unexplored but highly relevant subject about how digitization of health care might reconfigure basic social institutions. The main learning outcome is that digitalization matter beyond the individual patient provider- interactions. Digitalization might reconfigure social institutions. Among others, the study show how families and next of kin are essential for successful digital patient-provider interaction. This raises important questions about how digitized patient- provider interaction while the patients are at home relates to social inequality. Will digitalization increase social inequality? This discussion is particular relevant for the implementations areanas; Stavanger universitetssykehus: KOLS-kofferten; Sørlandet sykehus: United 4 Health and; Lyngby Taarbæk kommune: Epital.
In 2019, the WP8 researcher Lisbeth Kvam and Kari Dyb are working on two main publications. One, departing from NASSS (Nonadoption, Abandonment, Scale-Up, Spread and Sustainability (of Health and Care Technologies), a new implementation framework developed by Trisha Greenhalgh el at (2017). NASSS is an evidence-based, theory-informed, and pragmatic framework to help predict and evaluate the success of a technology-supported health or social care program. The NASSS framework included questions in seven domains: 1) the condition or illness, 2) the technology, 3) the value proposition, 4) the adopter system (comprising professional staff, patient, and lay caregivers), 5) the organization(s), 6) the wider (institutional and societal) context, and 7) the interaction and mutual adaptation between all these domains over time. The framework raise a variety of challenges across all seven domains, each classified as simple, complicated or complex, where programs characterized by complicatedness proved difficult but not impossible to implement, whereas those characterized by complexity in multiple NASSS domains rarely, if ever, became mainstreamed.
To help predict and evaluate the success of technology-supported health or social care program, we apply the seven NASSS domains on the empirical material from the four 3P innovations arenas, aiming to describe, compare and understand what it happening at the four different arenas. Based on the NASSS framework, we hope to provide site specific and general learning outcome suitable for discussion among the 3P members, and to contribute the theoretical debates within implementation science.
Preliminary findings show empirical similarities and differences between the four innovation arenas. Related to domain 1) the condition or illness, Universitetssykehuset Nord Norge HF: Pasintsentrert helstjenesteteam – PSHT- is more complex and include a wider range of multiple, dynamic and unpredictable conditions than the other arenas. On the other hand, in domain 2) the technology; we find limited variation. It seem like the different technologies are quite strait forward and work well at the three arenas where technologies are implemented. Domain 3) the value proposition; include both supplies side value to the developers, and the support side value to the involved patients. All four arenas communicate solely on patient value. It is our interpretation that the supply side value are less explicit and need development at all the innovation arenas. Domain 4) the adopter system; comprise professional staff, patient, and lay caregivers, and demonstrate satisfaction among users across most arenas. One arena might need development. Domain 5) the organization; includes the organisation’s capacity to; innovate, readiness for this technology, funding, extent of change, and the work needed to create change. Our empirical data, across all arenas illustrate how organisational change is challenging. To change established funding models in Scandinavian health and care services is not a simple task, but extremely complex. Domain 6) the wider institutional and societal context; relate to political/policy, regulatory/legal, professional and socio-cultural issues. Again, we find similarities between the four innovation arenas. However, we also find huge variations related to context complexity and which context cause implementation challenges at the different arenas. The last domain, domain 7) relatas to the interaction and mutual adaptation between all the domains over time. This is complicated and challenging at all arenas, a successful project phase is no guarantee for successful adoption.
The second paper has working title, “Health care providers’ visions about person centered: loyalty to the vision represented by key participants involved in an eHealth project”. Our ambition is to contribute to the understanding of the concept “Person centered care” by empirically investigate how health personnel involved in the different eHealth projects at the four innovation arenas communicate their personal vision of person centered care. By exploring differences and similarities between health care providers, innovation arenas, health care trusts and countries, we aim to identify the main discourses constituting the concept; Person centered care. This is work in progress. However, we have included as learning outcome - spring 2019 due to its relevance for involved health care providers. We want to challenge all the involved participants to reflection about their own visions about persons centered care. Have the visions changed over time? Are there differences between professions, locations or conditions?
Contacts
- Deede Gammon, senior researcher NSE, email hidden; JavaScript is required
- Eunji Lee, Postdoctor, OUS / University of Copenhagen, email hidden; JavaScript is required
Description of the interdisciplinary work package
Work Package 9 “Patient Experiences” aims to develop methods for eliciting, monitoring and assessing the implementation of services that are based on the following 3P principles from the perspectives of patients:
- From reactive to proactive and planned care;
- From diagnosis focused to combined evidence-based medicine and person-centered care;
- From fragmented single disease to coherent team-based care;
- From viewing patients as passive recipients to supporting the informed active patients’ role in their own care.
Objectives for the interdisciplinary work package
Our goal is greater insights and improved methods for ensuring the voice and needs of patients in care planning and conduct.
Completed data gathering activities in 2017 and 2018 for WP7 and WP9 (fieldwork)
See tables for this on WP 7.
Dissemination - Links and Publications
Eunji Lee, Lars Kayser, Deede Gammon, and Gro Berntsen. Engaging and empowering citizens with long-term conditions: How to define personal goals and how to support the goal achievement with technology? The 18th International Conference on Integrated Care (ICIC18). Link to presentation: https://drive.google.com/drive/folders/1G6QO4yTFb5wJEk9xEvRHtcZn4Ly8YYZk
Eunji Lee and Deede Gammon. Identifying Personal Goals of Patients with Long Term Condition: A Service Design Thinking Approach. Studies in Health Technology and Informatics 2017; Volume 244, P.93-97. DOI: 10.3233/978-1-61499-824-2-93. Available at: http://ebooks.iospress.nl/volu...
https://www.jmir.org/2017/5/e1... This recent publication from mental health care illustrates some of the approaches and methods we are working towards for people with multiple chronic conditions.
Learning outcomes 2017
Health personnel think it's meaningful to be able to work towards the patient’s personal goals.
Patients are not used to thinking about ‘what is important for them’. When we talked to them about it, they often provided thoughts on resources that can make life more meaningful (e.g., travel).
The participants (the health personnel in the project) think the service design methodological approach using the visual icons was very useful, inspiring and helpful to reflect on how they work in today’s practice. Throughout the group exercises, they could not only confirm that they are on the right track, but also get new ideas about how they want to work. They say it is very important to reflect on why and what to do differently.
Learning outcomes 2018/2019
The preliminary impression from fieldwork
- The service design method for the group work (focus group) worked well in Egersund, but without a patient participant. Is it difficult for patients to attend due to illness or distance? How can we increase patient participation in such group work?
- The sites find it difficult to recruit patient participants for their projects.
- There is a need for a systematic way of mapping personal goals (for example, categorization according to life domains: family and network, health, economy, home and daily life, leisure and education).
Preliminary findings from scoping review (full-text screening is now on the process)
- Few articles include personal goals or how they are identified/formulated.
- Personal goal types: Mainly related to behavioural changes, such as physical activity, diet, medicine intake, sleep, stress management, etc. Some also reported on personal life goals but very few.
- Who defined personal goals ?: In most cases, patients and healthcare professionals defined together.
- Who followed up? (case manager): Nurses, psychologists, mentors, GPs, nutritionists, physiotherapists, social workers, interdisciplinary teams, research assistants / research coordinators, apps, patients themselves
- Very few informal caregivers (for example, family and friends) were involved in those studies
Contacts
- Geir Sverre Braut, Professor, Stavanger University Hospital/University of Stavanger, email hidden; JavaScript is required, tel +47 51 51 37 76.
Description of the interdisciplinary work package
Safety assessments of pharmaceuticals are well established procedures in legislation and research as well as in clinical practice. Standards are even developed for testing medical equipment, but we still do not have any accepted standard or method for analysing safety and risk related to other technologies or new organizational concepts in clinical settings.
Safety assessments of pharmaceuticals are well established procedures in legislation and research as well as in clinical practice. Standards are even developed for testing medical equipment, but we still do not have any accepted standard or method for analysing safety and risk related to other technologies or new organizational concepts in clinical settings.
Objectives
In the first phase of the project we shall:
- Introduce the analytical model and its theoretical background for the researchers at the different sites that will be taking part in the project.
- Elaborate an initial risk picture based on generic and specific data relevant for each site/relevant WPs.
- Define risk indicators to be followed during the clinical studies.
The second phase will contain the following activities:
- Collecting data on how the selected risk indicators have been used during the operational phase.
- Extracting experiences on the pro’s et con’s of this approach as a means of clinical governance at local level.
Dissemination - Links and Publications
- Article: Establishing local risk pictures as basis for increasing safety and reducing risk when introducing new technologies in health care.
- Article: Experiences with a standardized method for safety assessment and risk analysis of innovations in clinical care.
- Article: Participation from the public and from patients when designing health services.
Learning outcomes 2018
The experiences so far indicate that the chosen model for risk assessment is usable in clinical practice. An article presenting the model and the use of it in Tromsø is under preparation. Late 2018 and early 2019 the working package will explore how user experiences and users’ interests can be included in developing risk picture.
Learning outcomes 2019
The model for risk assessment developed on basis of the project in Tromsø has been tested in relation to patients with chronic obstructive pulmonary disease acutely admitted to a primary health care nursing home.