A New Boost for Health Technology
Several large digitalization and technology projects in healthcare have faced setbacks. Now, there is optimism around smaller projects and incremental changes.

By freelancer Kristin Straumsheim Grønli
"I have great faith in the future," says Else Tobiassen, advisor at the Department of eHealth in The Norwegian Association of Local and Regional Authorities (KS).
KS has taken on an increasingly central role in ensuring the digitalization and modernization of the healthcare sector, including coordinating projects, providing guidance, and facilitating collaboration among municipalities in networks.
Several reports and studies offer hope that technology will help save society from challenges that could potentially lead to the collapse of the healthcare and welfare services.
Will to change
The number of elderly people is increasing significantly, which in turn raises the demand for services from an already highly pressured sector. The availability of labour is not increasing. The maths doesn't add up.
Healthcare professionals and their expertise must be utilized much more efficiently than before, and there will be fewer employees per patient, according to the Health Personnel Commission's public report “Tid for handling” (NOU 2023:4 – in Norwegian only).
The solutions to maintain or improve the quality of services involve investments in buildings, equipment, and digital solutions, as well as better task distribution and organization within the services, according to the report.
In the municipalities, Tobiassen experiences optimism about adopting health and welfare technology.
"We can partly thank the corona pandemic for this, as it led to the adoption of more digital solutions. But it's also about increasingly recognizing the vast opportunities," she says.

“Realise that they need to”
The optimism contrasts with the myriad of sad news reports about large, controversial e-health projects. Are the efforts to digitise and modernise health and care finally on track to speed up the transition?
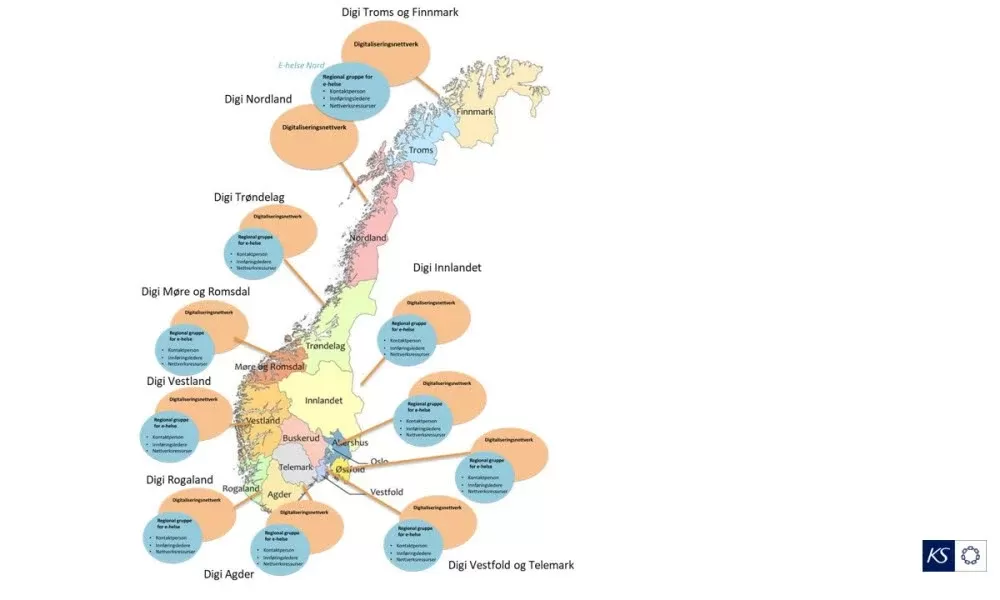
Together with the municipalities and Norsk helsenett (Norwegian Health Network), KS has just created a new model for the implementation of health technology and national e-health solutions. Here, municipal networks are central, in the form of regional groups for e-health.
The aim is to bring together expertise and skilled resources and ensure better coordination, capacity and support.
"The municipalities are willing to change things. They realise that they have to," says KS advisor Tobiassen.
She emphasizes that it is easier for the municipalities to understand the need for change when they can rely on and refer to research.
In the PROTECT network project, Nordic researchers have come together to promote and unite Nordic research-based knowledge about health and welfare technology. You can read some of their specific advice in two fact boxes in this article.
Fewer per patient
Although progress has been slow, more and more municipalities have acquired a range of technological tools to improve and ensure a sustainable health and care service.
This technology can enable the elderly to live at home longer, such as medication dispensers or digital supervision through sensors, GPS, or cameras. This is often referred to as 'welfare technology' or 'safety and mastery technology.'
It can also be technology that allows general practitioners and specialist health services to observe and follow up with a patient with a specific diagnosis while the patient is at home. Such solutions are often referred to as digital home monitoring.
The administration is now consolidating these terms under the designation 'health technology,' as the Welfare Technology Program transitions to the Health Technology Program starting in 2024.

Bottom-Up Approach
Since 2014, the National Welfare Technology Program has been a collaboration between KS, the Directorate of eHealth, and the Norwegian Directorate of Health, aimed at getting more municipalities to adopt such technology. The approach has consistently been quite bottom-up.
An important part of the program has been a grant scheme where municipalities and county municipalities have applied for support for procurement, implementation, and testing, but not for purchasing solutions.
Else Tobiassen at KS emphasizes that it is largely about helping municipalities with networking, methodology, and systematics for how they can proceed, without imposing strong guidelines on the work.
“We are a wealthy country. This allows for innovation and experimentation, instead of someone putting their foot down and deciding that everyone should go for one solution,” she says.
At the same time, it is important that municipalities learn from each other. Therefore, the work with municipal networks is also a very important part of the program.
Must be linked to medical records
Good electronic patient records and secure systems for information exchange are fundamental prerequisites for the digital and technological development of health and care services.
“The technology must be integrated with journal systems," says Line Helen Linstad, research fellow and senior adviser at the Norwegian Centre for E-health Research.
She is a political scientist and researcher on the public governance of e-health, focusing on the governance model that was established in the wake of the white paper "One citizen - one medical record" from 2013.

Since then, there has been a clear political goal that medical records should be able to follow patients through all the intricate pathways of the health and care services.
The fact that this goal has still not been achieved threatens patient safety and the possibilities for effective treatment, according to several plans and reports.
“A literature study I conducted shows that governance models in e-health are a combination of top-down processes, such as governmental ambitions, and bottom-up processes, such as medical needs,” says Linstad.
Finding a good balance between these different types of processes is no simple task.
“The healthcare sector has many strong stakeholders with power, money, and various systems. Attempting to exert governmental control is a difficult balancing act,” says Linstad.
Highly Criticized
In 2021, the Office of the Auditor General of Norway concluded that the work of both the Ministry of Health and Care Services and the Norwegian Directorate of eHealth had severe and highly criticized weaknesses.
Several key stakeholders, such as the Norwegian Medical Association, the Norwegian Nurses Organisation, and the industry, felt they were not adequately heard. The Office of the Auditor General concluded that the governance model was used more as a legitimization and consultation mechanism rather than a genuine consensus model.
Research communities also did not have significant influence on the national priorities in the assessment of “One Citizen – One Journal,” according to the Office of the Auditor General.
Key professional environments were not sufficiently involved, including the Norwegian Centre for E-health Research, the University of Agder, SINTEF, and the University of Oslo.
“It is possible that trust could have been maintained if there had been more public consultation rounds on the various reports that were produced,” says Linstad.
This aligns with the conclusion of the Office of the Auditor General that hearings on significant measures were underutilized.
“Now, the state has instead handed over the responsibility for managing the work with municipal records to KS and the municipalities themselves. They have to build this from the ground up,” says Linstad.
KS calls the project "Common Journal Initiative for Municipalities." Norsk Helsenett, the national service provider for e-health, is a collaboration partner.
Ecosystem
In addition to the fact that key parties were not adequately heard, the rapid technological developments that made open platforms and ecosystem solutions more relevant than large and complex packaged solutions were also not quickly enough recognized.
Today's consensus is that platform and ecosystem solutions are the future for the healthcare sector, according to the Office of the Auditor General.
These are systems that grow more organically and from the bottom up, while core systems ensure that data is shared securely. This supports innovation and an ecosystem of applications and services from many different providers, according to the Office of the Auditor General.
Bjørnar Alexander Andreassen is the acting director of the Department of Welfare Technology and Rehabilitation at the Norwegian Directorate of Health. He says there is now considerable practical experience showing that welfare technology can yield benefits in terms of both time saved for healthcare personnel and increased quality of services.
“Some of the large and expensive e-health projects have not delivered the expected outcomes. Now there is a renewed effort to take things more gradually with small development projects. We see that we have made some progress, but it is still too slow,” he says.

Benefits
Andreassen believes it is especially important for the research community to focus on the overall societal level to try to produce quantitative knowledge about potential benefits, such as time savings and cost reductions.
“This is the area where there has been the least amount of research so far,” he says.
Andreassen emphasizes the importance of having good data that documents both the implementations and the long-term costs and benefits for society. He believes this can be motivating at the political level.
“This makes it easier to feel confident about what we are investing in and focusing on. Today, we lack this overview. When we invest at one level – for example, welfare technology in municipalities – there is not enough information gathered to determine if this leads to benefits at another level, such as fewer hospital admissions,” he says.
The goal for patient records remains the same: patient information should be available to patients and healthcare professionals across all service levels.
Advice at the Societal Level
These are the PROTECT researchers' recommendations for health and welfare technology at the overarching societal level (see separate articles for the researchers' advice at the implementation and user levels):
Effects and Costs
- Build more knowledge about the effects, including costs and savings.
- Use quality-assured methods to build knowledge. Combine quantitative and qualitative approaches.
- Think broadly: implementing and examining a single solution is not enough. Large-scale knowledge projects covering the entire national ecosystem are needed.
- Broaden the perspective: how does the overall economic situation benefit from good health and welfare?
Systematic Reviews
- Conduct thorough, systematic reviews of existing knowledge. This is crucial for decision-makers.
- Create a clear categorization of solutions. This is necessary for systematic mapping and will make it easier to identify knowledge gaps.
- Identify knowledge gaps by involving various stakeholders.
- Conduct comparative studies, for example, between municipalities or countries.
Being Proactive
- Decision-makers must demonstrate national leadership and provide support for change management within organizations.
- Decision-makers can benefit from foresight activities such as scenario building and horizon scanning.
- Remember digital inclusion and the risk of exclusion: digital skills should not be taken for granted.
Source: Proactive health and welfare technology for Nordic users and societies - A policy brief
More Information (Norwegian):
- Tid for handling. Personellet i en bærekraftig helse- og omsorgstjeneste (NOU 2023:4)
- Riksrevisjonen: Undersøkelser av IT-satsingen Én innbygger –én journal; styring og anskaffelser: Dokument 3:14 (2020–2021)